Just over 3 weeks ago, on 19th Feb, I asked the wonderful social media world, and the health visitors who inhabit it, to help me in a quest. I wanted to find out where all the health visitors in England work. I outlined the reasons for this in another blog. I just wanted to give you a quick update as to the progress made!
By the 9th March, we had done it and cleared the first hurdle and found out who employed the health visitors in each English Council area. To make it easy for anyone who wanted to search the information, I also created a Google Sheet.
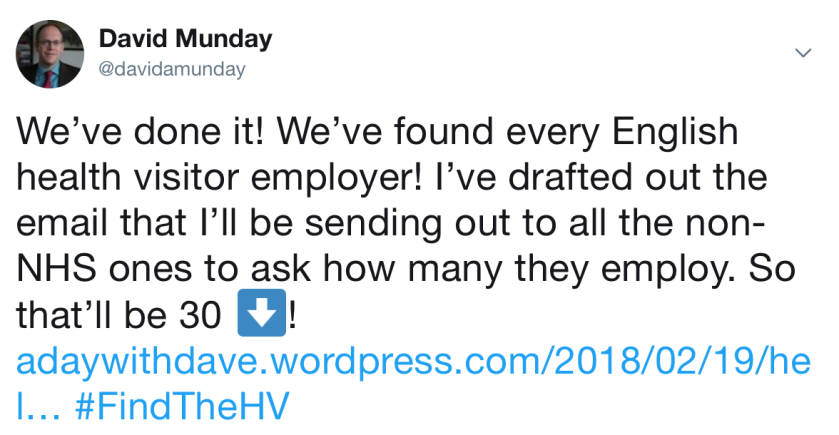
The next stage in my quest? To ask each the 30 non-NHS organisations a few questions that would help with finding out the true picture of health visitor numbers in England. I sent these emails on Tuesday (13th Feb). Here’s the text of what I sent (NB. the line about the Freedom of Information Act was only included to Councils as the others aren’t required to provide information under the Act):
Dear Sir/Madam,I am currently identifying how many health visitors there are in England. This information is already available for health visitors employed by NHS organisations (via NHS Digital). I am making requests of the other organisations that employ health visitors.Please can you provide me with:
- The number of health visitors that you employ? I have included the definition used by NHS Digital below, and I would be grateful if you could also use this definition. If you are unable to use this definition, please identify which definition you have used instead.
- The date that you started providing the health visitor service?
- The number of health visitors that were employed on the day of transfer?
If required, I’m asking for this information under the Freedom of Information Act.I will be posting all the responses to my blog, where I hope people will be better able to scrutinise the number of health visitors in England. You can read some more background to this here (https://adaywithdave.wordpress.com/2018/02/19/help-i-need-somebodies-health-visitors-help/).Regards,Dave Munday
…and here’s that very helpful NHS Digital definition:
Definition used by NHS Digital re. Health visitors (notes 28 and 29 from the nursing, midwifery and health visiting staff matrix of Occupation Code Manual)28. Please ensure to code the following as Health Visitors:
- qualified nurses/midwives who also hold a qualification as a Registered Health Visitor under the Specialist Community Public Health Nursing part of the NMC Register working directly with children and families;
- qualified and registered Health Visitors who perform specific activities such as providing breastfeeding advice to parents;
- family nurses working within the Family Nurse Partnership Programme who are qualified and registered as Health Visitors;
- Sure Start Children’s Centre qualified and registered named Health Visitors;
- managers within a Health visiting team who hold a health visiting qualification and registration and are involved in clinical work or safeguarding.
29. Please ensure that the following employees are not coded as Health Visitors:
- any person working in a health visiting team who does not hold a qualification and registration as a Health Visitor;
- any person who holds a qualification and registration as a Health Visitor but is not employed in a role where this is a requirement;
- managers within a health visiting team who hold health visiting qualification and registration but are not involved in clinical work or safeguarding.
Please see below the general definition for ‘health visitor’ from the Occupation Code Manual:Health Visitor: An employee who holds a qualification as a Registered Health Visitor under the Specialist Community Public Health Nursing part of the NMC Register and who occupies a post where such a qualification is a requirement. Not below Agenda for Change Band 6.
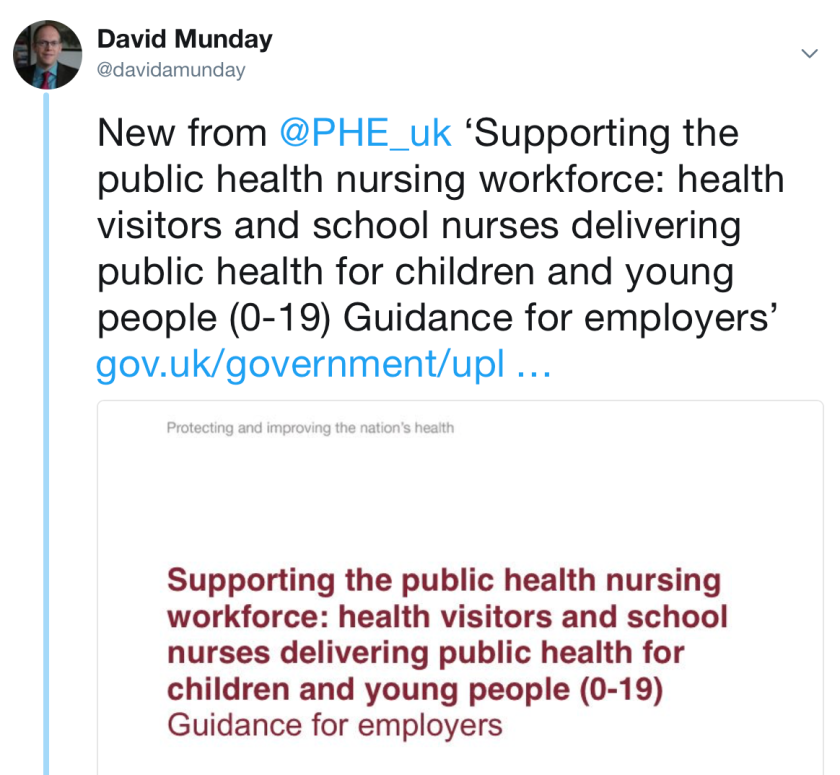
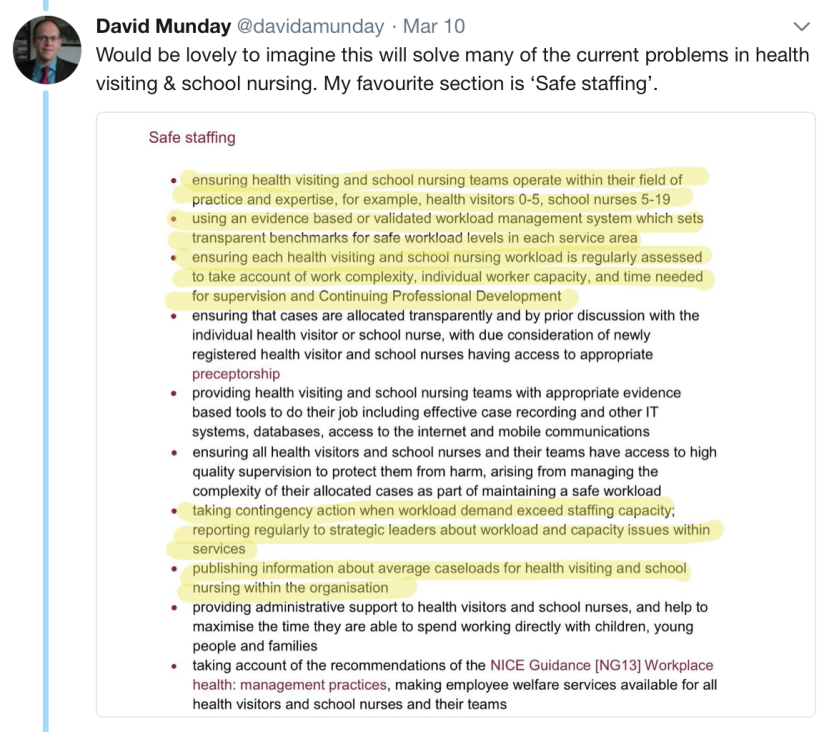
“publishing information about average caseloads for health visiting and school nursing within the organisation”




![Help, I need somebodies [health visitors] help!](https://adaywithdave.wordpress.com/wp-content/uploads/2018/02/img_3249.jpg?w=1200)