Today the House of Commons Health Committee have published their report on the nursing workforce inquiry. This brings to an end, a long process for the committee, which started last September. I’ve been involved with that process, contributing to the writing of the Unite in Health written evidence, supporting a colleague with their appearance in front of the committee to give oral evidence and following other aspects of the work. There’s a huge amount of material that can be shifted through on the inquiries website, including the final report which runs to 55 pages in length.
There are 17 conclusions and recommendations, across the 5 topics;
- Retention – keeping the current workforce
- New nurses
- Nursing associates
- Nurses from overseas, and
- Workforce planning
There’s worthy stuff in there, but before I look at some of this I wanted to address one of the big issues; nurses have been spectacularly failed by the current government, and here’s why…
Listening to Jeremy Hunt speak, he focuses on talking about the increase in ward nurses. A recent tweet he shared highlighted that in 1 year, there were ‘800 more nurses on wards’. There is truth in that statistic. In fact looking at the total number of nurses and health visitors in the NHS, we’ve seen a 2.2% increase in their number since 2010.

With all these figures you’ve got to remember that over a similar time period, the population in England has increased by 2.6 million, or 5%, so even a 2.2% increase is really a 2.8% ‘real terms’ cut.
Looking at adult nurses, the picture unusually shows one of an actual real terms increase. Their number has increased by 6.5% since May 2010 (before considering that population growth I’ve mentioned above).

When you go a little further down the NHS Digital spreadsheet however, things don’t look anywhere near as ‘marginally getting better’.
Community health nurses, well they’ve gone down by 14.7%…

Learning disability nurses, down by a staggering 37.4%….

School nurses, down by 20.1%….

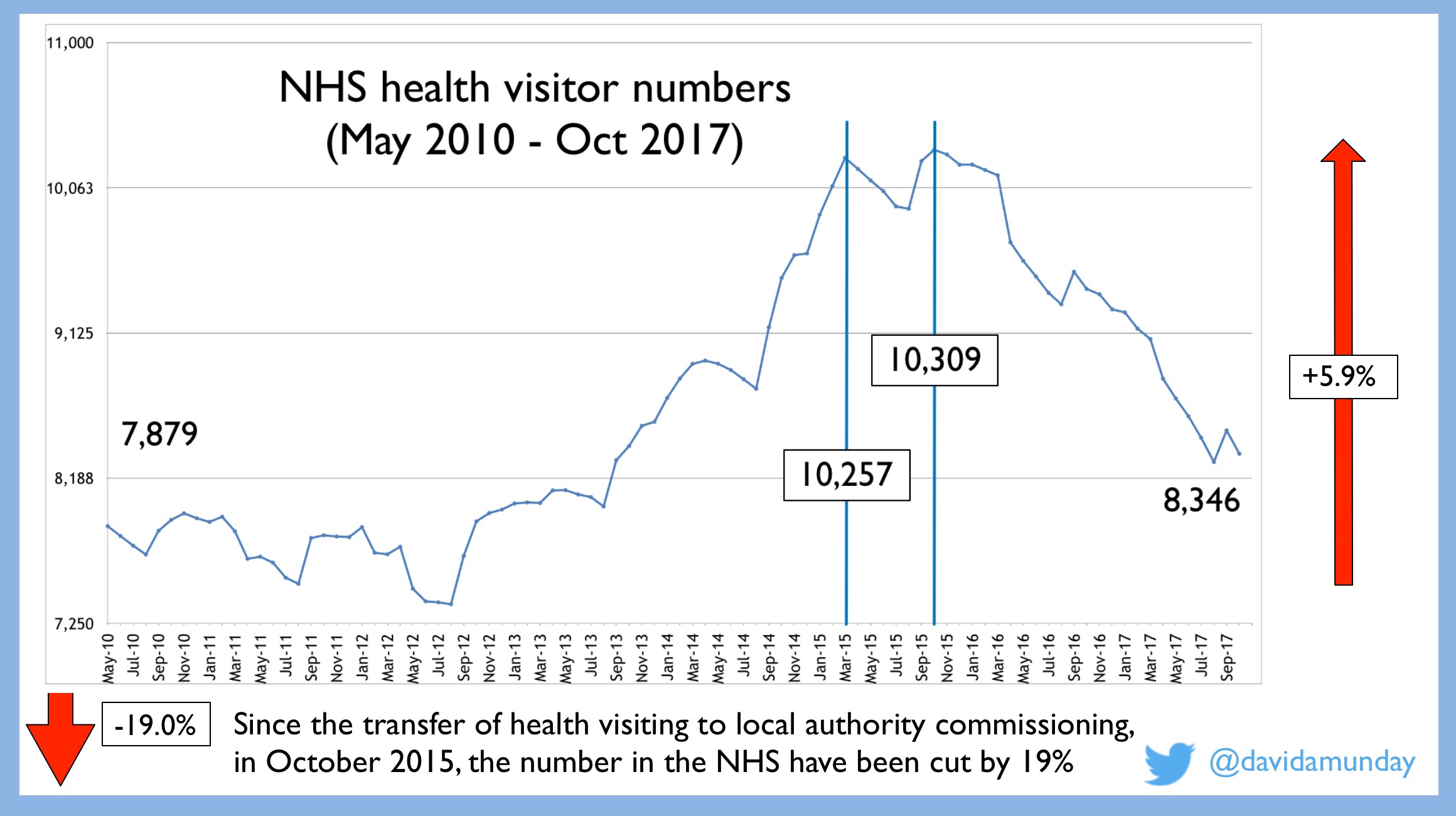
And although health visitors have seen a 5.9% increase, since their transfer from NHS to local authority commissioning, they’ve been cut in the NHS by 19.0%.
For mental health nurses, their number have reduced by 11.4%.

All these are despite warm words about the importance of community services, early intervention, mental health, et al. Is enough being done to alter their steep downward trajectories? Again, although we’re told there is, I think the proof is sorely lacking.
And these cuts to staff have great and grave impact on patients and service users. For example earlier this week, the Care Quality Commission, in their report, ‘Mental Health Act – The rise in the use of the MHA to detain people in England‘ identified that a growing number of people were being detained under the Mental Health Act due, in part, to gaps in support and provision.
The calamitous decision to remove NHS student bursaries for new students has seen a marked decline in the number of people putting themselves forward to run the education gauntlet. What’s even more perverse about this is that the report makes clear that this decision has impacted the choices made by those in older age groups, and in their graph on page 21, they show how these groups, aged 30 or over, make up a larger percentage of two of the nursing fields that are facing some of the worst drops in numbers, 39% in learning disability nursing and 40% in mental health (62).
The report talks about monitoring the bursary issue ‘very closely’ (71). As a colleague, Jane Beach says however, “…we don’t have the luxury of waiting another year to know how this will play out. The evidence of nursing shortages from NHS Digital is already stark and alarming”.
Thinking on Jane’s point about the luxury of time, as I’ve shown above, the cuts to many professions in nursing have been significant, constant and going back 7+ years. This long period of failing the professions means that the response now should be more immediate and have a greater impact. As in many things, I have no confidence that the Government will take the necessary action.
One area that our Mental Health Nurses Association have argued for is to have safer staffing legislation. Unfortunately the report does not make a recommendation on this. It should have.
Another recommendation that Unite made was to look to improve public protection by better protecting the nurse title. As Prof. Alison Leary uncovered in her recent research, the current situation is not fit for purpose. Again the report is silent.
One area that the report does encourage is more accurate data collection (115). This would be excellent. As I was reading this through I noticed an answer to a Parliamentary Question from Sir Nicholas Soames (MP), answered by Jackie Doyle-Price (MP), which suggests we’re heading in the wrong direction. When asked about health visitor numbers, the answer is now, one the one hand ‘we don’t know’ and on the other a misleading response given about ‘800 new training places being made available in 2016/17’. This is misleading as, was reported by Nicola Merrifield in the Nursing Times, one third of these courses places were left vacant.

There’s more that could be said about the report and its recommendations, for example I’ve not even got started on the issues of pay and retention rates. I’m getting tired though, as I’ve just got back from the NHS rally in London. As this report is on the nursing workforce, I wanted to give the final words to Siobhan, a specialist nurse, who spoke at the #NHSrally, as they seem fitting:
“Our NHS is not beyond repair… I believe it is our countries greatest achievement. We must and we will defend it”.













 Last week, I was lucky to attend the
Last week, I was lucky to attend the 
 In keeping with this, all of the keynotes had this thread running through them. As with any conferences, some sessions will stay with me longer than others. There were two that definitely stood out. My favourite of the whole event was delivered by Søren Dixen, a schizoform laywright, scholar of Nordic literature and a recovery-mentor at the Mental Health Services of the Capital Region of Denmark. He sessions focused on
In keeping with this, all of the keynotes had this thread running through them. As with any conferences, some sessions will stay with me longer than others. There were two that definitely stood out. My favourite of the whole event was delivered by Søren Dixen, a schizoform laywright, scholar of Nordic literature and a recovery-mentor at the Mental Health Services of the Capital Region of Denmark. He sessions focused on 


 The second keynote highlight was
The second keynote highlight was