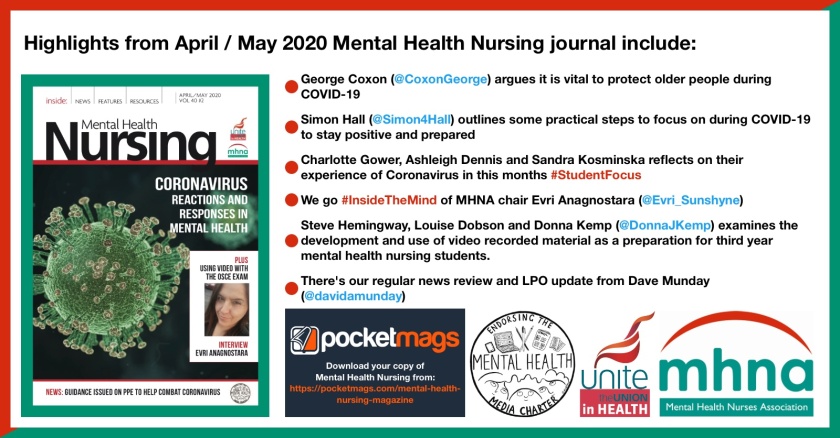
This update featured in the April/May 2020 Mental Health Nursing journal (Vol 40 #2). For those who aren’t Unite/MHNA members, you can buy your copy online via PocketMags or join and get 6 copies per year posted to your home and access to our back-issues online.
As I write this from my kitchen table on bank holiday Monday, now a scene of many a Microsoft Teams, Zoom, WebEx, GoToMeeting, Skype and WhatsApp Video over the last few weeks, it feels amazing that it’s only 25 days since my email to MHNA members to thank you for your efforts so far, in the battles against COVID-19.
So much has happened to our nation and our health service in such a short period of time.
In my responses to various people and organisations in recent weeks as your lead professional officer, I have repeatedly highlighted how we have entered a global pandemic with a much-weakened NHS and society.
It has struck after 10 years of austerity, where the poorest have suffered the most, and a mental health service that has faced cuts, including the 8.2% (between May 2010 and December 2019) drop in the number of mental health nurses working in England’s NHS.
While the government has taken dramatic action in some areas as a result of the pandemic, only time will tell whether this will be a continued change of heart after the initial impact of coronavirus is known.
Key areas of concern
There have been three key areas of concern that members have raised
the most frequently: the number of people working in the health service; the availability and supply of personal protective equipment to health service staff and other key workers; and the availability of COVID-19 testing for members of staff.
These are obviously all singularly important issues, but they also have a co-dependence on each other.
Alongside my role in supporting mental health nurses in Unite, I also have a role supporting our ambulance staff members.
Their concerns also highlight this co-dependency well. For example, one of our representatives has reported that her service, on that particular day, faced a 30% vacancy rate.
The rep providing the report was at home self-isolating as she had a new cough, and was feeling unsure whether she was infected, after having crewed her ambulance without the required range of PPE available.
PPE guidance
As you’ll see elsewhere in this edition, Unite has welcomed the updated PPE guidance issued by the UK public health organisations and the Academy of Medical Royal Colleges, although we remain acutely concerned about the levels of supply and distribution.
Unite has done a number of things including joining with the Trades Union Congress, alongside sister trade unions, to demand government action on this ‘crisis within a crisis’ – and has worked to repurpose members in manufacturing to use their skills, engineering and manufacturing expertise to ramp up production.
Collaborative working
Following requests from mental health professionals, we have been working with the Royal College of Nursing, the Royal College of Psychiatrists
and colleagues from NHS England to produce a poster resource specifically for mental health professionals.
Work on this is well under way, and it will hopefully be published well before this journal hits your doormat.
This has not been the only resources that we have joined together to work on. For the last few weeks we have been working on guidance across
a range of topic areas and services. These, and more, are all available from the Royal College of Psychiatrists’ website.
On this, I would like to offer my thanks to our lead reps from both MHNA and the Applied Psychology Organising Professional Committee, who have suffered the daily requests for feedback that I have made of them, alongside the jobs that they are doing in the NHS, the university sector and elsewhere.
Student views
This edition of the journal also picks out two other areas that have consumed time and effort.
It is great that we have been able to feature the reflections of three student nurses on how the coronavirus pandemic has impacted on them and their studies, so I send my thanks to the authors Charlotte, Ashleigh and Sandra for their insightful and thoughtful contributions.
Alongside my fellow lead professional officer and lead for regulation Jane Beach, I have been involved in regular discussions with the Nursing and Midwifery Council and others about the progress of changing students’ progress to registration.
Any questions should hopefully now be answered by the relevant guides in each of the four UK countries.
However, if any of our student nurse members have any questions, comments or concerns, please do not hesitate to get in touch with me.
Also, if you are a student then please consider sharing your experience and reflections on the coronavirus situation, and our regular Student Focus feature is the perfect publication opportunity for this. Email the editor via mhneditor@gmail.com if you would like to contribute.
If you want to hear more about our work for students, have a listen to episode one of our new series of The Mental Health Podcast.
The importance of mental health nurses
This issue of Mental Health Nursing also includes a welcome piece by Simon Hall from the University of the West of England, on the importance of mental health nurses, especially during the pandemic.
This has also been an area that has required much thought and consideration.
As in ‘normal’ times, people with mental ill health often get put to the back of the healthcare queue.
It would be a further travesty if this situation is furthered during COVID-19, with various attempts to divert mental health professionals to the ‘physical health fight’.
We have already opposed some plans that have been proposed nationally, which would have had exactly this impact.
Support is vital
It is clear that it will take a long time for the true impact of COVID-19 to become known.
What we know now, however, is that as well as a large death toll, the nation’s mental health will be impacted. And a significant part of this will be the mental health of key workers.
I was pleased to see that a national helpline has been launched for NHS staff in England. Alongside this resource, I would encourage all our members to ask for and get support when they need it.
This could mean phoning a helpline or talking with your colleagues, friends or family. It could also mean getting in touch with your local Unite workplace reps or contacting me.
Such support is vital, and we will all need these support mechanisms over the days, weeks and months ahead.
We also thought about some of these issues when putting together the second episode of season two of The Mental Health Podcast.
I wanted to finish this update by once again saying thank you for all that you are doing at such an exceptionally tough time.